Ever pondered the microscopic blueprint that dictates your very being? What if understanding this blueprint could unlock secrets to your health, ancestry, and even predispositions? DNA testing and genetic testing offer precisely that—a peek into the intricate world of your genome. This exploration, however, comes with a caveat: interpreting the vast amount of information requires careful consideration and expert guidance.
So, what exactly are DNA and genetic tests? And how do they differ?
Deciphering the Genetic Code: A Primer
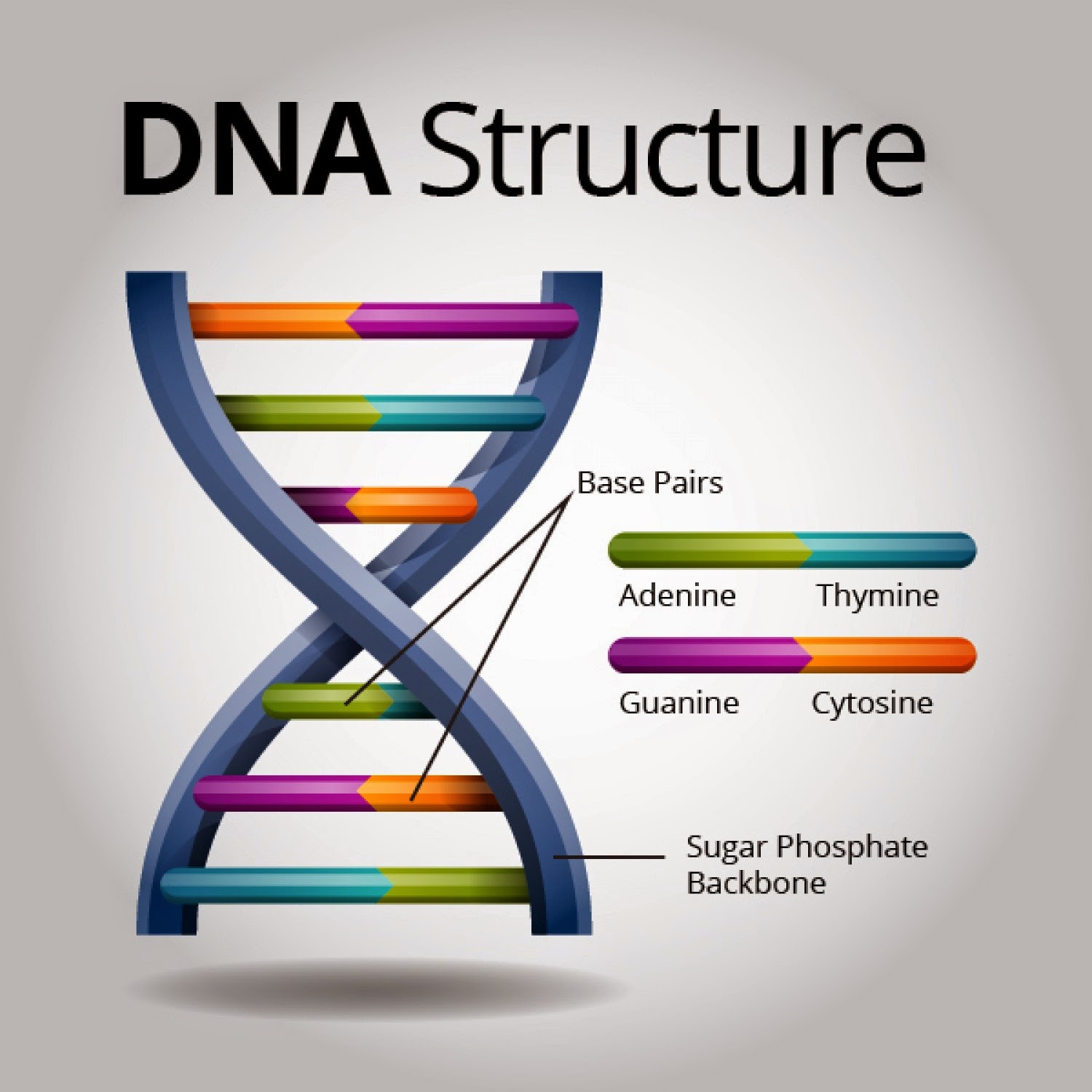
At its core, deoxyribonucleic acid (DNA) is the hereditary material in humans and almost all other organisms. It’s the instruction manual that governs our growth, development, function, and reproduction. These instructions are encoded within the double helix structure, composed of nucleotide base pairs: adenine (A) with thymine (T), and guanine (G) with cytosine (C). The sequence of these base pairs constitutes our genes. The human genome contains approximately 20,000 to 25,000 genes.
Genetic testing, on the other hand, is a broader term that encompasses various methods used to analyze DNA, RNA, chromosomes, or proteins to detect gene variations or abnormalities. These tests can identify changes that may cause disease or increase the risk of developing a disease. It is worth noting that the sensitivity and specificity of these tests vary greatly depending on the methodology employed.
Types of Genetic Tests: A Diverse Landscape
The realm of genetic testing is vast and constantly evolving. Several key types of tests are commonly used:
- Diagnostic Testing: This type of testing is used to confirm or rule out a suspected genetic condition in someone who is already showing symptoms. For instance, a child exhibiting developmental delays might undergo diagnostic testing to identify the underlying genetic cause. It provides concrete answers.
- Predictive and Presymptomatic Testing: These tests are utilized to identify gene mutations that increase a person’s risk of developing a disease in the future, even before symptoms appear. BRCA1 and BRCA2 testing for breast and ovarian cancer risk falls into this category. Huntington’s disease testing is a prime example of presymptomatic testing, where a positive result indicates that the individual will inevitably develop the disease.
- Carrier Testing: Carrier testing identifies individuals who carry one copy of a gene mutation for a recessive genetic disorder. While carriers typically don’t exhibit symptoms themselves, they can pass the mutation on to their children. This is particularly relevant for couples planning a family, as they can determine their risk of having a child with a condition like cystic fibrosis or sickle cell anemia.
- Prenatal Testing: Conducted during pregnancy, prenatal testing screens the fetus for certain genetic disorders, such as Down syndrome or trisomy 18. Chorionic villus sampling (CVS) and amniocentesis are invasive procedures that can provide definitive diagnostic information. Non-invasive prenatal testing (NIPT) utilizes maternal blood to screen for chromosomal abnormalities with high accuracy.
- Newborn Screening: This type of testing is performed shortly after birth to identify infants who may be at risk for specific genetic disorders that can be treated early in life. Phenylketonuria (PKU) and congenital hypothyroidism are common conditions screened for in newborns. Early detection and intervention can significantly improve outcomes.
- Pharmacogenomic Testing: This analyzes how a person’s genes affect their response to certain medications. This information can help healthcare providers choose the right medications and dosages for each individual, maximizing efficacy and minimizing adverse effects. For example, variations in the CYP2C19 gene can affect how individuals metabolize clopidogrel, a common antiplatelet drug.
- Ancestry Testing: This is perhaps the most widely known type of genetic testing. It analyzes DNA to provide insights into a person’s ethnic origins and genetic relationships. While entertaining and informative, it’s important to remember that ancestry testing relies on statistical probabilities and may not always provide a complete or definitive picture.
The Process: From Sample to Results
The process of genetic testing typically involves several key steps. First, a sample is collected, which can be blood, saliva, hair, skin, or amniotic fluid. Then, DNA is extracted from the sample and analyzed using various techniques. These techniques might include polymerase chain reaction (PCR) to amplify specific DNA sequences, DNA sequencing to determine the exact order of nucleotide bases, or chromosomal microarray analysis to detect deletions or duplications of large segments of DNA.
The results of genetic testing are then interpreted by a qualified healthcare professional, such as a geneticist or genetic counselor. It is important to consider the clinical context, family history, and other relevant factors when interpreting these results. Genetic counselors play a crucial role in helping individuals understand the implications of their genetic test results and make informed decisions about their health care.
Ethical Considerations and Potential Pitfalls
While genetic testing offers tremendous potential, it also raises significant ethical considerations. Privacy concerns are paramount. Who has access to your genetic information, and how is it protected? Genetic discrimination, where individuals are treated unfairly based on their genetic predispositions, is another serious concern. For example, employers or insurance companies might discriminate against individuals with genetic risks for certain diseases. The Genetic Information Nondiscrimination Act (GINA) in the United States provides some protection against genetic discrimination, but its scope is limited.
Furthermore, the interpretation of genetic test results can be complex and challenging. False positives and false negatives can occur, and even when a genetic mutation is identified, its clinical significance may not always be clear. Genetic variants of uncertain significance (VUS) are frequently encountered, leaving individuals and healthcare providers in a state of ambiguity.
Finally, the psychological impact of genetic testing should not be underestimated. Learning about a genetic predisposition to a disease can cause anxiety, fear, and depression. Genetic counseling is essential to help individuals cope with the emotional challenges associated with genetic testing.
Looking Ahead: The Future of Genetic Testing
The field of genetic testing is rapidly evolving, driven by technological advancements and a growing understanding of the human genome. Whole-genome sequencing, which involves mapping the entire genome, is becoming more accessible and affordable. Liquid biopsies, which analyze circulating tumor DNA in blood samples, are revolutionizing cancer diagnosis and treatment monitoring. Gene editing technologies, such as CRISPR-Cas9, hold the promise of correcting genetic defects, although ethical and safety concerns remain.
Ultimately, genetic testing empowers individuals with knowledge about their health and ancestry. However, it is crucial to approach genetic testing with caution, informed consent, and the guidance of qualified healthcare professionals. Only then can we harness the full potential of this powerful technology while mitigating its risks.








Leave a Comment