Ever feel like you’re surrounded by acronyms you only vaguely understand? PCR. It’s a term that’s been bandied about quite a bit lately, especially in the context of healthcare. But beyond the buzzwords and clinical settings, what exactly *is* a PCR test? What secret does this molecular magnifying glass hold? Forget the jargon for a moment. Think of PCR as a highly specialized detective, capable of finding the tiniest clues at a crime scene – clues so minuscule they’d be invisible to the naked eye.
This detective, armed with cutting-edge technology, isn’t searching for fingerprints or footprints. It’s on the hunt for genetic material – DNA or RNA. Why is this important? Because these genetic blueprints are the defining characteristics of…well, everything. From viruses and bacteria to the very cells that make up your body.
Let’s unpack that a bit further. This exploration will cover:
- The Basic Principle: Imagine making copies, not of documents, but of specific pieces of DNA.
- What a PCR Test Actually Detects: The difference between detecting the presence of a pathogen and diagnosing a disease.
- The PCR Process: Delving into the cycles of heating and cooling that underpin the entire operation.
- Applications Beyond Diagnostics: From forensic science to evolutionary biology, the surprising versatility of PCR.
- Limitations and Caveats: Understanding the potential for false positives and false negatives.
- The Future of PCR Technology: Exploring new innovations and advancements in the field.
The Basic Principle: Amplification is Key
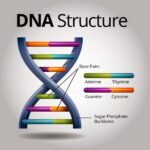
At its core, PCR, or Polymerase Chain Reaction, is a method of “amplifying” a specific DNA sequence. Imagine you’re trying to find a single, specific sentence in a library containing millions of books. Good luck, right? Now, imagine you have a machine that can automatically find that sentence and make billions of copies. Suddenly, your search becomes significantly easier. That’s essentially what PCR does.
The process relies on an enzyme called DNA polymerase. This enzyme is the workhorse of DNA replication, naturally occurring in cells. In a PCR reaction, the polymerase is harnessed to create new copies of the target DNA sequence. This amplification process occurs in a series of cycles, each doubling the amount of target DNA. A few initial molecules can quickly become billions, making them easily detectable.
What a PCR Test Actually Detects: Presence vs. Disease
Crucially, a PCR test doesn’t necessarily tell you if you *have* a disease. It tells you if the genetic material of a specific pathogen – a virus, bacteria, or other microorganism – is *present* in your sample. Think of it this way: finding a burglar’s footprint at your house proves he was there, but it doesn’t tell you if he stole anything.
A positive PCR result indicates the presence of the pathogen’s genetic material. However, the clinical significance of that finding depends on several factors, including the concentration of the pathogen (viral load, for example), the individual’s symptoms, and their medical history. You might test positive for a virus but never develop symptoms, or you might be in the early stages of an infection before the virus has had a chance to fully establish itself. Conversely, a negative PCR result suggests the pathogen is not present, or is present in such low concentrations that it’s undetectable. It doesn’t necessarily mean you are completely disease-free. There’s a “detection threshold”.
The PCR Process: Cycles of Thermocycling
The PCR process involves a series of temperature changes – “thermocycling” – that drive the amplification reaction. Each cycle typically consists of three steps: denaturation, annealing, and extension.
Denaturation involves heating the DNA sample to a high temperature (around 95°C) to separate the double-stranded DNA into single strands. Annealing involves cooling the sample (typically to 50-65°C) to allow short DNA sequences called primers to bind to the target DNA. These primers act as starting points for the DNA polymerase. Extension involves heating the sample to an optimal temperature for the DNA polymerase (usually around 72°C) to extend the primers and create new copies of the target DNA. Each cycle doubles the number of target DNA molecules, leading to exponential amplification.
Applications Beyond Diagnostics: A Molecular Swiss Army Knife
While PCR is widely used in diagnostics, its applications extend far beyond healthcare. In forensic science, PCR can be used to amplify DNA from minute samples, such as a single hair follicle or a drop of blood, to identify suspects or victims. In evolutionary biology, PCR can be used to study the genetic relationships between different species. In environmental science, PCR can be used to detect and identify microorganisms in soil or water samples. The possibilities are vast.
Limitations and Caveats: Room for Error
PCR is a powerful tool, but it’s not infallible. False positives can occur if the PCR reaction is contaminated with extraneous DNA. False negatives can occur if the sample contains inhibitors that interfere with the PCR reaction, or if the pathogen is present in very low concentrations. The technique is also susceptible to primer-dimer formation, where the primers bind to each other instead of the target DNA.
The Future of PCR Technology: Innovation on the Horizon
The field of PCR technology is constantly evolving. New innovations are aimed at improving the speed, sensitivity, and accuracy of PCR tests. Real-time PCR, for example, allows for the quantification of DNA during the PCR reaction, providing more precise results. Digital PCR offers even greater precision by partitioning the PCR reaction into thousands of individual reactions. These advances promise to further expand the applications of PCR in diagnostics, research, and beyond. The molecular detective is only getting more sophisticated.









Leave a Comment