Ever ponder if your genes hold secrets to your breast cancer risk? It’s a pertinent query, especially given the increasing awareness surrounding genetic predispositions to various diseases. The specter of hereditary breast cancer looms large for some, while for others, it’s a negligible concern. Ascertaining where you stand requires a nuanced understanding of genetic testing and its implications. This exploration delves into the critical factors that determine the necessity of genetic testing for breast cancer.
Family History: Unraveling the Genealogical Tapestry
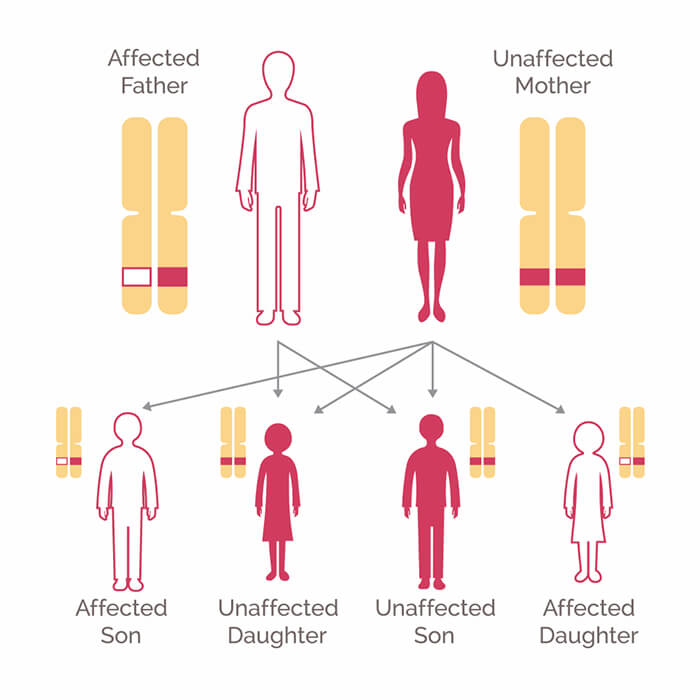
Your family’s medical chronicle is paramount in this deliberation. A strong family history of breast, ovarian, fallopian tube, or peritoneal cancer can signal a heightened risk. This isn’t merely about one distant relative; it involves a cluster of diagnoses across multiple generations, particularly among first-degree relatives (parents, siblings, children) and second-degree relatives (grandparents, aunts, uncles). The age of diagnosis also matters. Early-onset cancer, diagnosed before the age of 50, suggests a possible genetic component. Furthermore, the presence of rare cancers like male breast cancer or triple-negative breast cancer within the family further strengthens the case for genetic testing. Assessing the lineage with a thorough, detailed overview will reveal more details.
Ethnicity: Certain Ancestries, Elevated Risks
Specific ethnicities demonstrate a higher prevalence of certain gene mutations linked to breast cancer. Ashkenazi Jewish individuals, for example, have a significantly elevated risk of carrying BRCA1 and BRCA2 mutations. These genes, when mutated, drastically increase the likelihood of developing breast, ovarian, and other cancers. While other ethnic groups can certainly carry these mutations, the incidence is statistically higher in this population, making genetic testing a more pressing consideration. Understanding ancestral roots is crucial in risk assessment.
Personal History: Facing a Prior Diagnosis
If you have already been diagnosed with breast cancer, genetic testing might still be beneficial. It can inform treatment decisions and help assess the risk of developing a second primary cancer. For instance, knowing you carry a BRCA mutation might lead to more aggressive surgical options, such as a bilateral mastectomy, or influence the choice of chemotherapy regimens. Furthermore, it can provide valuable information for family members, enabling them to make informed decisions about their own health and preventive measures. A prior diagnosis does not eliminate the need for further investigation.
Understanding the BRCA Genes and Beyond
The BRCA1 and BRCA2 genes are the most well-known players in hereditary breast cancer, but they are not the only ones. Other genes, such as TP53, PTEN, ATM, CHEK2, and PALB2, also contribute to increased risk. These genes play crucial roles in DNA repair, cell growth, and other cellular processes. Mutations in these genes can disrupt these processes, leading to uncontrolled cell proliferation and cancer development. Comprehensive genetic testing panels can assess multiple genes simultaneously, providing a more complete picture of an individual’s genetic predisposition.
What Does Genetic Testing Involve?
Genetic testing typically involves a blood sample or a saliva sample. The sample is sent to a laboratory where it is analyzed for specific gene mutations. The results can take several weeks to come back. It’s important to note that genetic testing is not a diagnostic test for cancer; it only identifies an increased risk. A positive result does not guarantee that you will develop cancer, but it does mean that you should take proactive steps to manage your risk. Conversely, a negative result does not eliminate the risk of cancer, as many cases are not hereditary. There are limitations to every test.
The Psychological and Emotional Considerations
Genetic testing is not without its emotional baggage. Receiving a positive result can be overwhelming, leading to anxiety, fear, and uncertainty. It can also impact family relationships, as individuals grapple with the implications for their relatives. Conversely, a negative result can bring relief but may also create a false sense of security. It’s crucial to have access to genetic counseling before and after testing to help navigate these emotional complexities. Genetic counselors can provide support, answer questions, and help individuals make informed decisions about their health.
Risk Reduction Strategies: Taking Control of Your Health
If you test positive for a gene mutation, several risk reduction strategies can help mitigate your chances of developing breast cancer. These include: increased surveillance with mammograms and MRI scans, prophylactic surgery (mastectomy or oophorectomy), and chemoprevention (taking medications like tamoxifen or raloxifene). The optimal strategy depends on individual factors, such as age, personal medical history, and family history. Regular consultation with a healthcare professional is essential to tailor a personalized risk reduction plan.
The Role of Genetic Counseling
Genetic counseling is an integral part of the genetic testing process. A genetic counselor can assess your risk, explain the benefits and limitations of testing, interpret your results, and provide guidance on risk reduction strategies. They can also help you navigate the emotional and psychological aspects of testing. It’s important to choose a qualified and experienced genetic counselor who can provide comprehensive and personalized care. Counselors are invaluable resources.
Conclusion: A Personalized Decision
Deciding whether or not to undergo genetic testing for breast cancer is a deeply personal decision. It requires careful consideration of your family history, ethnicity, personal medical history, and emotional preparedness. Weigh the benefits against the potential risks and limitations, and seek guidance from healthcare professionals and genetic counselors. By understanding your own unique risk factors, you can make an informed decision that empowers you to take control of your health and well-being. The answer differs from person to person.








Leave a Comment