The question of whether clinical pathologists perform autopsies is a nuanced one, often shrouded in misconceptions. To understand it fully, we must first appreciate the distinct, yet interconnected, realms of clinical pathology and anatomical pathology. Think of them as two wings of the same majestic bird, each vital for its flight, yet possessing unique plumage and purpose.
The Two Pillars of Pathology: A Tale of Two Disciplines
Pathology, in its broadest definition, is the study of disease. It seeks to understand the mechanisms, progression, and manifestations of illness at the molecular, cellular, and tissue levels. However, the sheer breadth of this endeavor necessitates specialization. This is where clinical and anatomical pathology diverge.
Clinical pathology, sometimes referred to as laboratory medicine, focuses on the analysis of bodily fluids, such as blood, urine, and cerebrospinal fluid. Clinical pathologists are the orchestrators of the diagnostic laboratory, utilizing sophisticated instrumentation and complex assays to provide clinicians with crucial data for diagnosis, monitoring, and treatment. Their domain is the microscopic world of cells and molecules circulating within the body. A vast array of tests fall under their purview, including hematology (blood cell analysis), clinical chemistry (analyzing chemical components in fluids), microbiology (identifying infectious agents), and transfusion medicine (managing blood transfusions).
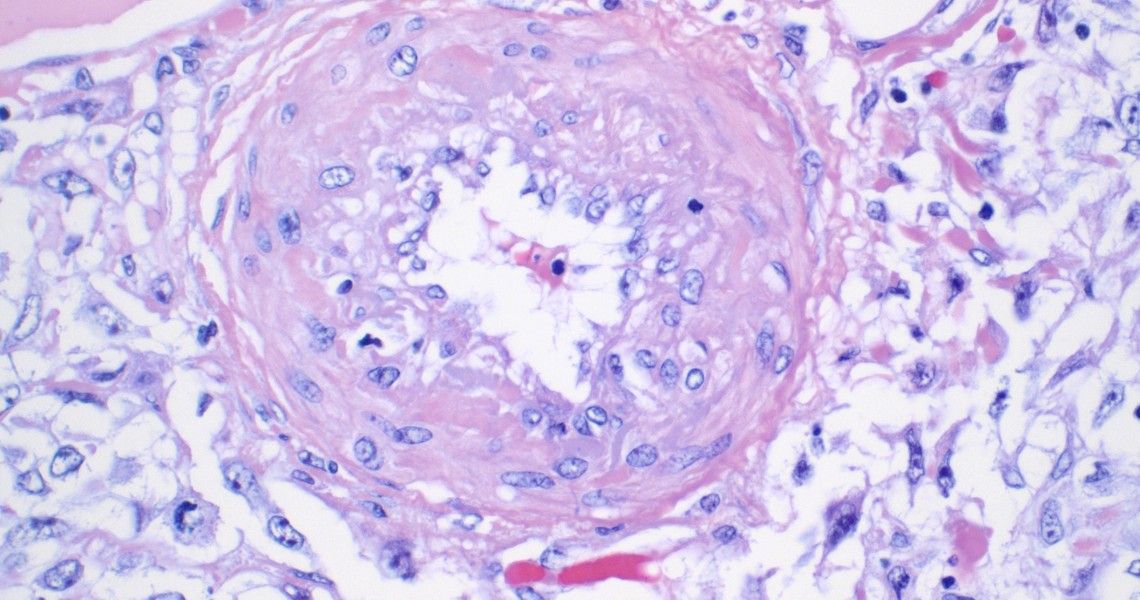
Anatomical pathology, on the other hand, deals with the examination of tissues and organs. Anatomical pathologists are the detectives of disease, meticulously examining biopsies, surgical specimens, and, importantly, conducting autopsies to determine the cause of death. They employ both macroscopic (naked eye) and microscopic techniques, using their profound knowledge of tissue architecture and cellular abnormalities to identify disease processes. Their reports guide surgical decisions, cancer staging, and the understanding of disease pathogenesis.
Autopsy: A Window into the Body’s Secrets
An autopsy, also known as a post-mortem examination, is a surgical procedure performed on a deceased person to determine the cause of death, manner of death (natural, accidental, suicide, homicide, or undetermined), and the presence of any disease or injury. It is a vital tool for understanding disease processes, improving medical knowledge, and ensuring public health. Consider it a final, meticulous physical examination, a last opportunity to learn from the body’s narrative.
The Role of the Anatomical Pathologist in Autopsy
The primary responsibility for performing autopsies rests squarely with anatomical pathologists. These specialists possess the requisite training and expertise in gross and microscopic examination of tissues, allowing them to accurately identify abnormalities and correlate them with the clinical history. They are adept at dissecting the body, examining organs, and collecting tissue samples for further analysis, such as histology (microscopic examination of tissue sections) and toxicology (detecting drugs or toxins).
Do Clinical Pathologists Ever Participate in Autopsies?
While anatomical pathologists are the primary conductors of autopsies, clinical pathologists may play a supporting, albeit less direct, role. Their expertise in laboratory testing can be invaluable in certain cases. For instance, if an autopsy reveals signs of infection, a clinical pathologist may be consulted to perform microbiological cultures to identify the causative organism. Similarly, if there is suspicion of drug overdose or poisoning, a clinical pathologist with expertise in toxicology may be involved in analyzing blood or tissue samples.
The interplay between clinical and anatomical pathology can be likened to a symphony orchestra. The anatomical pathologist is the concertmaster, leading the performance, while the clinical pathologist is a key section leader, providing crucial support and expertise to enhance the overall harmony.
Bridging the Divide: Overlapping Skill Sets and Collaborative Opportunities
It is important to acknowledge that the boundaries between clinical and anatomical pathology are not always rigid. Some pathologists choose to become board-certified in both disciplines, acquiring expertise in both laboratory testing and tissue examination. These “double-boarded” pathologists are uniquely positioned to bridge the gap between the two fields and provide comprehensive diagnostic services.
Moreover, collaborative efforts between clinical and anatomical pathologists are increasingly common. In complex cases, a multidisciplinary approach, involving both specialties, can lead to a more accurate diagnosis and a better understanding of the disease process. This synergistic approach highlights the interconnectedness of the two disciplines and the value of collaboration in modern pathology practice.
In Conclusion: A Division of Labor, United by Purpose
While clinical pathologists do not routinely perform autopsies, their expertise in laboratory testing can be invaluable in certain cases, providing crucial information that complements the findings of the anatomical pathologist. The division of labor between these two disciplines reflects the vast scope of pathology and the need for specialized expertise. Ultimately, both clinical and anatomical pathologists share a common goal: to understand disease and improve patient care. Their collaboration ensures a comprehensive and nuanced approach to diagnosis and the pursuit of medical knowledge, even in the face of death. They are, after all, united by the same Hippocratic oath and a shared dedication to unveiling the mysteries hidden within the human body.








Leave a Comment